Delve into the Impact of Your Diet on Triglyceride Levels in the UK
How do high-sugar foods lead to increased triglyceride levels in British diets?
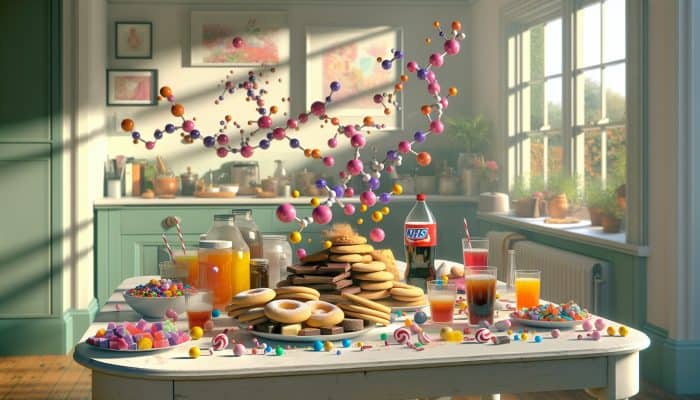
Understanding Triglycerides: High-sugar foods significantly contribute to the rise of triglycerides in British diets, particularly through the consumption of popular snacks such as biscuits, sweets, and sugary beverages. The UK’s National Health Service (NHS) recommends that added sugars should comprise no more than 5% of daily energy intake to mitigate health risks linked to elevated triglyceride levels. Recognising the widespread nature of these dietary practices is crucial for individuals who aim to maintain balanced lipid levels and overall health.
The habitual consumption of sugary snacks can lead to insulin resistance and metabolic syndrome, both of which are conditions that can further elevate triglyceride levels. The relentless availability of high-sugar foods in UK supermarkets and convenience stores exacerbates this issue, making it essential for individuals to actively monitor their sugar consumption and make healthier choices.
Moreover, British children are particularly vulnerable due to their high intake of sweets and fizzy drinks, which can result in long-term health complications. In response, schools and community initiatives are starting to address these dietary challenges by advocating for healthier snack alternatives. This education is vital in guiding the younger generation towards understanding the significance of maintaining healthy triglyceride levels.
 How does the consumption of fatty foods affect triglyceride levels in the UK?
How does the consumption of fatty foods affect triglyceride levels in the UK?
Traditional high-fat meals commonly found in British cuisine, such as fish and chips and full-fat dairy products, can significantly elevate triglyceride levels. The intake of saturated fats is a primary contributor to increased lipid levels, prompting the NHS to encourage individuals to select healthier fat alternatives, such as:
- Olive oil
- Avocado
- Fatty fish like mackerel
- Low-fat dairy products
These alternatives not only enhance the taste of meals but also provide essential nutrients that are beneficial for heart health. Incorporating these healthier fats into everyday meals can have a profound impact on lipid profiles, leading to healthier triglyceride levels.
Adopting a balanced approach to dietary fat consumption allows individuals to enjoy traditional British dishes while prioritising cardiovascular well-being. Understanding which sources of dietary fats are advantageous is crucial, as not all fats are detrimental. Both polyunsaturated and monounsaturated fats can actually help lower triglycerides, making it imperative for UK residents to distinguish between healthy and unhealthy fats in their dietary selections.
What are the patterns of alcohol intake among Britons and their effects on triglycerides?
Excessive alcohol consumption is a prevalent aspect of the UK pub culture, significantly impacting elevated triglyceride levels. Regularly consuming large quantities of alcohol can cause liver damage, impairing the organ’s ability to metabolise fats, which leads to higher triglyceride levels in the bloodstream. British health surveys indicate that binge drinking has become an alarming trend among adults, correlating with rising triglyceride levels.
The NHS advises that individuals should limit their alcohol intake to no more than 14 units weekly to mitigate the risk of elevated triglycerides and related health issues. Additionally, reducing alcohol consumption not only benefits lipid profiles but also enhances overall health and well-being. Raising awareness about the dangers of heavy drinking is critical, as community initiatives aimed at promoting responsible drinking can significantly help individuals manage their triglyceride levels while still enjoying social interactions without compromising their health.
How do processed foods impact triglyceride levels in the UK?

Processed foods, which are prevalent in British households, negatively affect triglyceride levels. Items like ready meals and crisps often contain high amounts of refined carbohydrates and unhealthy fats, both of which can elevate triglyceride levels. The NHS recommends limiting the intake of processed foods to enhance cardiovascular health and lower triglyceride concentrations.
Many processed foods are loaded with sugars and sodium, factors that further exacerbate lipid-related health concerns. Individuals should be vigilant about the nutritional content of these foods and strive to replace them with fresher alternatives, such as fruits, vegetables, and whole grains, which promote better health outcomes. Cooking at home using whole ingredients not only aids in managing triglyceride levels but also fosters healthier eating habits within families.
Emphasising whole foods in the diet can lead to improved health and well-being for individuals and families throughout the UK.
How does lifestyle influence triglyceride levels?
What is the significance of exercise in managing triglycerides for adults in the UK?
Exercise plays a pivotal role in managing triglyceride levels among adults in the UK. Engaging in regular physical activities, such as walking in local parks or joining group fitness classes, can lead to significant reductions in triglyceride concentrations. The UK government recommends that adults partake in at least 150 minutes of moderate-intensity exercise weekly to promote cardiovascular health and maintain optimal lipid profiles.
Participating in aerobic activities has been shown to enhance the body’s fat metabolism, effectively reducing triglyceride levels. Local communities provide a multitude of options, from jogging groups to cycling clubs, encouraging individuals to stay active while fostering social connections. This social aspect of exercise not only aids in managing triglycerides but also boosts mental health, further enhancing overall well-being.
Additionally, incorporating resistance training into one’s exercise routine can yield beneficial results. Activities such as weight lifting or bodyweight exercises strengthen muscles and increase the metabolic rate, which can help manage triglyceride levels. A well-rounded fitness plan tailored to individual preferences can ensure long-term adherence and success in controlling triglyceride levels.
What are the prevalent sedentary habits in the UK?

Sedentary habits, such as those associated with desk jobs or excessive television viewing, represent concerning trends in the UK. Such lifestyles significantly contribute to elevated triglyceride levels by reducing energy expenditure and disrupting metabolic processes. Public Health England highlights the critical need to reduce sedentary time to combat rising lipid levels.
Incorporating small lifestyle changes, like standing while working or taking regular breaks to walk, can counteract the negative impacts of prolonged sitting. Engaging in active leisure pursuits, such as gardening or outdoor sports, can further reduce sedentary behavior while promoting a more active lifestyle.
Moreover, communities are increasingly recognising the importance of active living, with local councils advocating initiatives designed to enhance physical activity. These efforts inspire residents to integrate more movement into their daily routines, transforming their lifestyle habits to improve health outcomes, including better triglyceride levels.
How does stress affect triglyceride levels in the UK?
Daily stressors, especially those related to work pressures in bustling British cities, can lead to elevated triglyceride levels through various biological mechanisms. Stress triggers the release of hormones like cortisol, which can result in fat accumulation and increased triglyceride synthesis. This relationship underscores the importance of effective stress management for maintaining healthy lipid profiles.
Resources from UK mental health organisations recommend several coping strategies to alleviate stress, including mindfulness, yoga, and consistent physical activity. Engaging in these practices can effectively reduce stress levels and positively influence triglyceride concentrations.
Support networks, whether through family, friends, or local community organisations, can provide essential emotional support during stressful periods. Encouraging open dialogues about mental health can significantly enhance overall well-being and contribute to healthier triglyceride levels, making it essential for individuals to prioritise their mental health alongside their physical health.
Insights from Experts on Factors Contributing to Increased Triglycerides
What do UK studies reveal about dietary influences on triglyceride levels?
Numerous British studies have highlighted how specific dietary choices impact triglyceride levels. A comprehensive analysis of NHS trials demonstrated that individuals consuming high quantities of refined carbohydrates exhibited significantly higher triglyceride levels compared to those prioritising whole grains and fibre-rich foods. This knowledge emphasises the crucial role that dietary choices play in effectively managing lipid levels.
To lower triglycerides, individuals can take actionable steps, such as replacing white bread with wholemeal alternatives, increasing their intake of fruits and vegetables, and minimising sugary snacks. Research indicates that these dietary changes can result in substantial improvements in lipid profiles.
Moreover, community-based interventions aimed at promoting healthier eating habits, such as food workshops and cooking classes, have produced positive outcomes by encouraging individuals to adopt diets that support healthy lipid levels. Such grassroots efforts are vital in addressing the growing concern of elevated triglycerides in the UK.
What insights do experts provide on lifestyle factors affecting triglycerides in the UK?
Analysis by UK health authorities indicates that sedentary lifestyles substantially contribute to elevated triglyceride levels. Data shows that individuals who do not engage in the recommended levels of physical activity are more likely to experience higher lipid concentrations. Experts advocate for a multi-faceted approach to tackle this issue, focusing on exercise, dietary habits, and stress management.
Implementing minor lifestyle changes can have a significant impact. For example, choosing active modes of transport like cycling or walking can drastically reduce sedentary time while enhancing cardiovascular health. Additionally, addressing dietary habits through community programs can reinforce the importance of a heart-healthy diet.
Practical advice from health professionals suggests that a comprehensive strategy that combines regular physical activity, balanced nutrition, and stress-reduction techniques can effectively manage triglyceride levels. Emphasising these strategies will empower UK residents to take proactive steps towards maintaining healthier lipid profiles.
What strategies should individuals with genetic predispositions consider in the UK?
For those genetically predisposed to elevated triglycerides, personalised strategies are essential for effective management. British genetic research indicates that inherited factors can significantly influence lipid metabolism. Nevertheless, lifestyle modifications can help mitigate these risks. Collaborating with healthcare providers enables individuals to develop tailored NHS plans that address both genetic and lifestyle factors.
Implementing dietary changes, such as increasing omega-3 fatty acids from sources like fatty fish or flaxseeds, can counteract genetic tendencies towards elevated triglycerides. Regular monitoring of lipid levels, alongside genetic counselling, can provide insights into individual risks and management strategies.
Moreover, community initiatives that promote genetic awareness can empower individuals to take charge of their health. By understanding their genetic risks, residents can make informed choices specifically targeting triglyceride management, fostering a proactive approach to cardiovascular health.
What health conditions are associated with high triglycerides?
How does obesity influence triglyceride levels in the UK population?
Obesity has become an escalating concern in the UK, with rising rates closely linked to increasing triglyceride levels. Studies indicate that excess body fat, particularly around the abdomen, correlates with higher triglyceride concentrations. The connection between obesity and elevated triglycerides underscores the necessity for effective weight management strategies to prevent cardiovascular diseases.
The NHS has identified obesity as a significant risk factor for numerous health conditions, including type 2 diabetes and heart disease, both of which are exacerbated by high triglycerides. Effective prevention strategies emphasise healthy eating and consistent physical activity, highlighting the need for comprehensive lifestyle adjustments.
Community health initiatives focused on addressing obesity through education and support can significantly lower triglyceride levels across populations. By promoting healthier behaviours, residents can combat the rising obesity rate and its associated health risks.
What is the link between diabetes and triglycerides in British demographics?
The relationship between type 2 diabetes and elevated triglycerides is particularly pronounced within British demographics. Individuals with type 2 diabetes often experience dyslipidaemia, characterised by high triglycerides and low HDL cholesterol levels. Understanding this connection is crucial for effectively managing overall health.
- Obesity
- Physical inactivity
- Unhealthy diet
- Family history of diabetes
According to the British Diabetic Association, managing triglycerides is a vital aspect of diabetes care, as high levels can increase cardiovascular risks. Implementing dietary modifications alongside regular exercise can significantly enhance lipid profiles in people with diabetes, ultimately improving their health outcomes.
Supporting individuals in understanding their condition and the importance of triglyceride management is essential. Community support programmes can offer valuable resources, enabling individuals to take proactive steps toward better health.
What is the connection between heart disease and triglycerides in the UK?
High triglycerides are a significant factor in the development of cardiovascular diseases, making them a critical public health concern in the UK. Elevated triglyceride levels are often associated with an increased risk of heart attacks and strokes, as they contribute to the hardening and narrowing of arteries.
UK health campaigns have focused on raising awareness about the importance of monitoring triglyceride levels as part of overall heart health. These initiatives emphasise the necessity of regular health checks and lifestyle modifications to maintain healthy lipid profiles.
Implementing strategies to lower triglycerides, such as adopting a Mediterranean-style diet rich in fruits, vegetables, and healthy fats, can significantly improve cardiovascular outcomes. Community initiatives aimed at educating the public about heart health can influence awareness and encourage healthier lifestyle choices.
How are triglycerides linked to hypertension in the UK?
Elevated triglycerides are closely associated with hypertension among British adults. Research from the Health Survey for England shows that individuals with high triglycerides frequently experience elevated blood pressure, creating a concerning cycle that heightens cardiovascular risks.
The NHS advises lifestyle modifications, including dietary changes and regular physical activity, to manage both triglyceride levels and blood pressure. Emphasising the importance of a heart-healthy diet and effective stress management can significantly improve health outcomes for individuals at risk.
Community support and educational initiatives focused on hypertension and triglyceride management can empower residents to take proactive steps to reduce their cardiovascular risk. By fostering healthier lifestyles, individuals can effectively manage both conditions.
What associations exist between high triglycerides and liver disease in the UK?
High triglycerides are linked to non-alcoholic fatty liver disease (NAFLD), a condition prevalent in Britain. Increased triglyceride levels can lead to fat accumulation in the liver, resulting in inflammation and potential liver damage over time. Public Health England underscores the importance of monitoring triglycerides as part of liver health assessments.
Dietary interventions play a crucial role in managing triglyceride levels and promoting liver health. The British Liver Trust recommends adopting a balanced diet rich in whole foods, minimising saturated fats and sugars, and increasing physical activity to enhance liver function.
Community awareness campaigns focused on liver health can greatly impact public understanding of the risks associated with high triglycerides. Educating residents on maintaining healthy triglyceride levels is vital for preventing liver disease.
What are the research-backed benefits of managing triglycerides?
What key findings emerge from UK research on lipid control?
Research from British institutions has shown that effectively managing triglycerides can lead to significant health improvements. Studies indicate that individuals with lower triglyceride levels face a reduced risk of developing cardiovascular diseases and metabolic disorders. These findings underscore the importance of regular monitoring and proactive management of triglyceride levels.
Experts assert that lifestyle modifications, including healthy dietary choices and increased physical activity, are vital for lipid control. The long-term health benefits of maintaining optimal triglyceride levels are substantial, leading to a better quality of life.
Community health initiatives promoting triglyceride management provide essential resources for residents. By raising awareness of the connection between triglycerides and overall health, individuals can make informed decisions to better manage their lipid levels.
What effective interventions have been proven in UK trials?
Clinical research in the UK has identified successful interventions for managing triglycerides, particularly through dietary modifications. Trials reveal that adopting a diet rich in omega-3 fatty acids, found in fish and flaxseeds, can significantly lower triglyceride levels. These findings offer actionable steps for individuals looking to improve their lipid profiles.
Moreover, engaging in regular physical activity has proven beneficial. Research indicates that even moderate exercise can effectively reduce triglyceride levels, emphasising the importance of a balanced lifestyle. Community fitness programmes designed to promote physical activity can enhance the effectiveness of these interventions.
By understanding the evidence-based strategies that yield positive results, residents can take charge of their health and make informed dietary and lifestyle choices to manage triglyceride levels effectively.
What lifestyle modifications have proven effective in UK studies?
Evidence from British trials shows that simple lifestyle changes can lead to significant reductions in triglyceride levels. Participants who adopted a Mediterranean diet, rich in fruits, vegetables, whole grains, and healthy fats, experienced notable improvements in their lipid profiles. This dietary pattern not only supports heart health but also contributes to overall well-being.
Additionally, increasing physical activity levels has been shown to enhance triglyceride management. Studies suggest that regular exercise, whether through structured workouts or daily activities, can effectively lower lipid levels and improve cardiovascular health.
As communities embrace these lifestyle modifications, support programmes promoting healthy choices will be instrumental in achieving better health outcomes for residents across the UK.
What is the role of medication in triglyceride control based on UK research?
Research from British clinical trials has explored the effectiveness of medications in lowering triglyceride levels, particularly statins and fibrates. These medications have demonstrated the ability to reduce lipid levels, effectively improving cardiovascular health. However, experts emphasise the importance of combining medication with lifestyle changes for optimal results.
Patients should consult their healthcare providers to determine the most suitable approach for managing triglycerides, encompassing medication options and lifestyle adjustments. This comprehensive strategy can optimise lipid profiles and mitigate associated health risks.
Community healthcare initiatives focused on educating residents about the role of medication, along with health-promoting behaviours, can enhance overall health outcomes and improve the quality of life for individuals managing elevated triglycerides.
Why is consistent monitoring of triglyceride levels crucial?
What signs should individuals in the UK be vigilant about?
Individuals in the UK should stay alert to common symptoms of high triglycerides, which may not always be readily apparent. Symptoms can include unexplained fatigue, abdominal discomfort, and chest pain. Regular health check-ups through the NHS are essential for identifying these issues early and facilitating prompt intervention to manage triglyceride levels effectively.
Furthermore, monitoring cholesterol levels and overall cardiovascular health can provide vital insights into an individual’s risk profile. Understanding these symptoms and the necessity of regular check-ups is key to proactive health management.
Community health campaigns aimed at raising awareness about these symptoms can empower individuals to seek medical advice, ultimately leading to improved health outcomes across the population.
When is it advisable to consult a GP in the UK?
Consulting a GP is crucial when individuals notice symptoms such as persistent fatigue, abdominal pain, or if they have a family history of high triglycerides. Early intervention is critical because elevated triglyceride levels can lead to serious health complications. The NHS recommends regular screenings for individuals at risk, especially those with obesity or pre-existing health conditions.
Seeking medical advice can provide insights into managing triglyceride levels through lifestyle changes, dietary adjustments, or necessary medications. Awareness of personal health and proactive engagement with healthcare professionals can greatly improve health outcomes.
Community resources can aid individuals in understanding when to seek help and how to maintain healthy triglyceride levels, fostering a culture of proactive health management.
What are the long-term effects of unmanaged triglyceride levels on British health?
The long-term effects of uncontrolled triglycerides can be severe, leading to increased risks of cardiovascular diseases, diabetes, and liver complications within the British population. Longitudinal studies reveal a clear correlation between high triglyceride levels and negative health outcomes over time.
Preventive measures, including regular monitoring and lifestyle changes, are crucial for mitigating these risks. The NHS advocates for education and awareness campaigns to inform residents about the importance of proactively managing triglycerides.
Community initiatives that promote healthy behaviours can significantly reduce the long-term impact of elevated triglycerides on public health.
What benefits arise from early detection through regular monitoring?
The early detection of high triglycerides through routine monitoring can effectively prevent serious health issues in the UK. Regular health checks via the NHS provide critical insights into lipid levels, enabling timely interventions for effective triglyceride management.
Understanding one’s health status empowers individuals to make informed choices regarding their diet and lifestyle, ultimately leading to improved health outcomes. Community health initiatives that emphasise the significance of regular check-ups can cultivate a culture of proactive health management.
Encouraging residents to prioritise routine screenings is vital in preventing long-term health complications associated with high triglycerides.
How can monitoring be integrated into daily routines in the UK?
Integrating triglyceride monitoring into daily life is essential for UK residents seeking better health. Practical methods include tracking dietary intake and physical activity, which various mobile applications and health resources can facilitate. The NHS provides guidelines to help individuals maintain a balanced lifestyle while keeping an eye on their lipid levels.
Setting achievable health goals, such as increasing physical activity or reducing sugar intake, can make regular monitoring more manageable. Engaging with local health initiatives can also provide invaluable support and resources for those aiming to effectively manage their triglycerides.
By prioritising health monitoring as part of daily routines, residents can take proactive steps to maintain optimal triglyceride levels and foster long-term well-being.
Effective Prevention Strategies for UK Residents
What are the healthy eating guidelines endorsed by British sources?
The NHS endorses various healthy eating guidelines that are crucial for maintaining triglyceride levels, focusing on balanced meals characteristic of UK cuisine. Residents are encouraged to incorporate a diverse range of fruits, vegetables, whole grains, and lean proteins while limiting saturated fats and added sugars.
Emphasising the importance of portion control and mindful eating can further support healthy triglyceride levels. Community-based nutrition programmes can assist individuals in making informed dietary choices that align with these guidelines and contribute to overall cardiovascular health.
By fostering awareness about the benefits of healthy eating, residents can implement positive changes that significantly enhance their triglyceride levels and overall well-being.
What physical activity recommendations does the UK provide?
Physical activity recommendations from Public Health England highlight the importance of engaging in regular exercise suitable for British weather and lifestyle. Residents are encouraged to participate in activities such as walking, cycling, and swimming to boost cardiovascular health and effectively manage triglyceride levels. A typical weekly routine may include:
- 30 minutes of brisk walking five times a week
- Two sessions of strength training
- Weekend sports activities
- Daily active commuting
Local community centres and parks offer numerous opportunities to engage in physical activity while enjoying social connections. Establishing a supportive environment encourages individuals to stay active and incorporate exercise into their daily routines, yielding positive effects on triglyceride levels.
By promoting active living, communities can cultivate a culture of health that benefits all residents, leading to improved overall health outcomes.
How important are regular health check-ups through UK services?
Routine health check-ups through NHS services are vital for monitoring triglyceride levels and overall health. The NHS recommends that individuals, particularly those at risk, participate in regular screenings to identify potential issues early.
Incorporating these check-ups into daily life can help maintain awareness of one’s health status. Residents are encouraged to schedule appointments for regular assessments, including lipid profiles and blood pressure checks, as part of their health management strategies.
Community health initiatives that stress the importance of regular screenings can empower individuals to prioritise their health, fostering a proactive approach to triglyceride management and overall well-being.
Frequently Asked Questions
What are triglycerides?
Triglycerides are a form of fat (lipid) found in your blood that serves as an energy source for your body. Elevated levels can increase the risk of heart disease and other health complications.
How can I lower my triglyceride levels?
Lowering triglyceride levels can be achieved through lifestyle modifications, such as adopting a healthy diet, increasing physical activity, and maintaining a healthy weight.
What foods should I avoid to manage triglycerides?
Avoid foods that are high in sugar, refined carbohydrates, and unhealthy fats, such as sugary snacks, white bread, and fried foods, to help manage your triglycerides effectively.
How often should I have my triglyceride levels checked?
It is advisable to have your triglyceride levels checked at least once every five years, or more frequently if you possess risk factors such as obesity or diabetes.
Can exercise aid in reducing triglycerides?
Yes, regular exercise can significantly lower triglyceride levels. Aim for at least 150 minutes of moderate-intensity exercise each week for optimal results.
Is alcohol consumption linked to triglyceride levels?
Yes, excessive alcohol consumption can elevate triglyceride levels. It is crucial to drink in moderation to maintain healthy lipid levels.
What role does weight play in triglyceride levels?
Excess body weight, particularly around the abdomen, corresponds with elevated triglyceride levels. Losing weight can markedly improve lipid profiles.
Does genetics influence triglycerides?
Yes, genetics can affect triglyceride levels. If there is a family history of high triglycerides, it is vital to monitor your levels and adopt healthy lifestyle practices.
What are the symptoms of high triglycerides?
High triglycerides often do not present noticeable symptoms, but they can lead to complications such as abdominal pain or fatigue. Regular health checks are essential for detection.
How can I enhance my diet to manage triglycerides?
Focus on a balanced diet abundant in fruits, vegetables, whole grains, and healthy fats. Limit sugar and processed foods to manage triglyceride levels effectively.
Connect with Us on Facebook!
This Article Was First Found On https://bloodtest.co.uk
The Article Triglycerides Increase: Key Causes and Associated Risks Was Found On https://limitsofstrategy.com

